A mutant stink bug bites a retired scientist while he soaks in the tub, setting off a cascade of events. Fatigued and sporting a small red sore, the scientist heads off to bed. He awakens the next morning to a festering wound—the hallmark of a bacterial infection. The scientist has in his possession a shoebox-sized DNA sequencing device and biologic printer, and swabbing his infection site reveals the culprit: a strain of a flesh-eating bacterium. He springs into action, quickly manufacturing a life-saving cure.
This is the hypothetical scenario put forward by Belgian microbiologist Jean-Paul Pirnay in a paper he wrote in Frontiers in Microbiology in 2020. The article, titled “Phage Therapy in the Year 2035,” imagines a patient narrative to discuss the crux of Pirnay’s research: using viruses to fight off bacterial infection. In a surprising twist of cosmic justice, these viruses, called bacteriophages or phages for short, infect bacteria much in the same way bacteria infect us. That part isn’t science fiction. Phages occur all over nature, floating in our oceans, teeming in soils and sewers, coexisting with us in our own guts—but identifying, designing, and delivering these viruses to the people who most need them has proved an aspirational goal. So far.
Naturally-occurring bacteriophages that infect and burst bacteria with extremely high specificity fall somewhere between an evolutionary oddity and an inevitability.
Bacteriophages are the heroic counterparts to the modern-day supervillainy that is widespread antibiotic resistance. Each virus is the result of coevolution, a highly choreographed lockstep with a single strain or even substrain of bacteria. Similar to how every species of fig tree has its own pollinating wasp, it’s thought that every species of bacteria has at least one phage that infects it.
Drug resistance is currently far outpacing the discovery of new antibiotics, and clinical development has actually been slowing down compared to just five years ago, according to the World Health Organization. Part of the crisis, according to pharmaceutical companies, is that taking a new antibiotic from discovery to approval is simply not profitable. A bill called the PASTEUR Act, first introduced in Congress in 2020 and reintroduced this April, would shake up the compensation scheme for antibiotic development, but its passage is by no means guaranteed.
Even if the bill does pass, it won’t change the fact that people in the U.S. contract more than 2.8 million antibiotic-resistant infections every year. Drug resistance isn’t a looming specter—it’s right here, right now.
Dozens of people have been treated with phage therapy, and at least four universities have established dedicated phage therapy centers to keep up with growing demand for near-intractable, antibiotic-resistant infections. In many of those cases, phage therapy has done the improbable. One therapy saves a person’s life when all other treatments fail. Amid a worsening crisis, alternatives like phage therapy might be one of our best hopes, if not our only one.
Bacteriophages have been a mainstay in medical centers abroad for some time now. Georgia’s Eliava Institute has been active since the 1930s. Yet countries including the U.S. and U.K. grant access almost exclusively under compassionate use. That means bacteriophages have been languishing for decades as a last-ditch option.
In 2016, Tom Patterson became the first person in the U.S. to receive IV phage therapy for his antibiotic-resistant infection of Acinetobacter baumannii. His wife, Steffanie Strathdee, a University of California, San Diego epidemiologist, worked with scientists and regulators to save his life. Researchers from the Navy and a Texas A&M lab pinpointed several phages that neutralized samples of the bacteria taken from Patterson’s infection, and after a green light from the Food and Drug Administration, their phage cocktail coursed through his veins. Three days later, Patterson awoke from a coma. He’s since completely recovered.
It’s often only the sickest patients who get the treatment, and only in the end stage of their disease. In that sense, proponents say it’s remarkable that phage therapy has had meaningful impacts for these patients at all. They believe that countless lives would be saved if it were used earlier—and more often.
Paul Garofolo, the CEO of Locus Biosciences, a pharmaceutical company developing phage therapies, suggests that one day, they could become our drug of choice against superbugs and common bacteria alike. With phage therapy, “there’s a viable path to replacing antibiotics for humanity,” he says. This common sentiment—something akin to a religious fervor, really—drives academic researchers and startup founders to push phage therapy forward.
What few seem to agree on, though, is which road to take. Expanding grassroots networks. Democratizing phage research. Fighting an uphill battle to validate phage therapy in clinical trials. All are on the table. Ultimately, it may come down to one’s worldview: When a system is broken, do you try to fix it or start from scratch?
Bacteriophages are the heroic counterparts to the modern-day supervillainy that is widespread antibiotic resistance.
Small, Yet Mighty
Bacteriophages are the most abundant lifeform on Earth by a factor of 100; we’ve only discovered a fraction of the 10 nonillion (that’s 31 zeroes) of them—a vast, unknown ocean of clinical possibility. But when microbiologist Jessica Sacher researched phages in graduate school at the University of Alberta in the 2010s, she recalls being taught to ridicule researchers who believed phage therapy could work at the clinical level. “I remember so strongly being like, ‘Don’t get caught dead believing in phage therapy,’” she says.
The first documented use of phage therapy occurred in 1919, when French microbiologist Felix d’Herelle gave a mixture of phages to a boy with severe dysentery (d’Herelle imbibed the cocktail first, deeming it safe). The boy recovered and European scientists kept researching phages until the advent of antibiotics. Though Soviet Bloc scientists continued to study and use phages, the Iron Curtain isolated them and chilled intercontinental collaboration.
By the middle of the 20th century, viruses had taken a backseat to indiscriminate, broad-spectrum synthetic drugs. Early experiments underwhelmed as phages didn’t seem effective enough against pathogens, and researchers struggled to purify enough phages to make a potent dose. Phage therapy, scientists argued, would never scale. This thinking has persisted, as Sacher notes, despite new evidence challenging those early misconceptions.
Sacher’s perspective changed after seeing a Tweet in 2017 about Mallory Smith, a 25-year-old in Pittsburgh who was fighting an antibiotic-resistant Burkholderia cepacia infection. The bacteria had spilled into her bloodstream, causing life-threatening sepsis. Strathdee—who had saved her husband’s life with phage therapy the year prior—took to Twitter to ask phage researchers for viruses that could infect Burkholderia cepacia.
A researcher from Canada replied to Strathdee, offering to send phages that fight Smith’s infection. That researcher didn’t belong to a fancy, hospital-affiliated clinical lab. They were an academic—and, in fact, they worked in a lab that Sacher previously neighbored: “They were a lab like ours, with grad students who each had a little phage project,” Sacher says. And they weren’t the only ones who volunteered.
A day after tweeting, Strathdee replied with an update that several phage labs had agreed to help Smith in her fight against the antibiotic-resistant infection. Meanwhile, Smith wasn’t doing well; her septic fever rose to 106 degrees at one point, and she contracted a fungal infection on top of the Burkholderia superbug. Antibiotic resistance, Smith wrote, was “a complex, unpredictable, irreversible, progressive, painful, suffocating, choking weed.”
Sacher told Jan Zheng, a bioinformatics engineer she’d met through swing dancing, about Smith’s case and her unexpected connection to it. Zheng gravitated toward the story for a different reason. He saw that doctors needed experimental phage treatments as more and more bacteria outsmarted last-line antibiotic defenses. Meanwhile, hundreds of labs worldwide studied phages, and some had private libraries of thousands of strains. Individual scientists who had cumulatively cataloged a vast supply of phages needed some way to collaborate in order to meet the urgent demand. Phages needed a matchmaking platform at an international scale. The pair created that site, called Phage Directory, in November 2017.
Despite researchers and clinicians working around the clock, Smith passed away from her Burkholderia infection the same month. “That was crystallizing for us,” Sacher says. “It made us think: this is a real life and death thing.” She wonders what might have happened had researchers identified candidate phages and gotten compassionate use approval.
Smith’s mother was more explicit. In a May 2023 blog post for the Centers for Disease Control and Prevention, she wrote: “If Mallory had gotten phage therapy sooner, she could have lived.”
Since its founding, Phage Directory has sent out 50 alerts to its community of global researchers on behalf of patients who, like Smith, have no other option. They’ve had a handful of success stories. There was a young girl in Australia whose legs became infected with Pseudomonas aeruginosa after a car crash. Twelve labs responded to an alert by shipping candidate phages to Australia. A cocktail of them all cured the infection, saving the girl’s legs.
The Australian girl’s case converted Sacher’s side project into her career. She now works in Sydney as a postdoctoral fellow designing a country-wide phage therapy system. The system is the first of its kind, but Sacher admits it faces tough challenges. “Phage therapy is not hard if you do it for one person,” she says. “It’s very hard if you try to scale it up and do it for lots of people. That’s what’s hamstrung our field.”
Going Global
The phages that populate biologists’ growing catalogs frequently come from the last place you’d want to look. Raw sewage is an ideal source of diverse bacteria and, with any luck, the wild phages infecting them, explains Tobi Nagel, founder and president of Phages for Global Health.
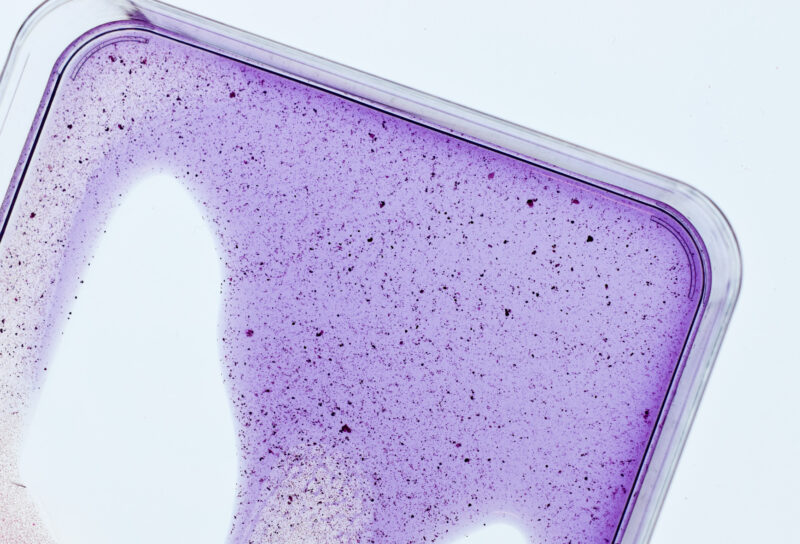
The organization holds regular workshops where participants sample sewage from a local plant. After filtering the samples, the 25 or so scientists in attendance add them to petri dishes containing “lawns” of Escherichia coli and Pseudomonas bacteria. By the next day, they start to see small pockmarks on the lawns—a sign that phages are present and killing off colonies of bacteria.
Nagel and her team at Phages for Global Health have run these workshops since 2017 in low- and middle-income countries, spurred by the disproportionate burdens these countries face from antibiotic resistance. By 2050, projections suggest, nearly 89 percent of deaths caused by resistant microbes will occur in Africa and Asia. But while antibiotic-resistant infections are skyrocketing, antibiotic drug development is stalling.
Antibiotic discovery thrived from the 1940s to the 1960s, after scientists realized that antibiotic-producing microbes lived abundantly in soil. Probing underground soon ran out of steam, though, and labs developed zero new classes of antibiotics between 1962 and 2000. Progress has remained slow: In 2021, there were just 27 new antibiotics in clinical development against the World Health Organization’s list of priority pathogens, down from 31 in 2017. Large pharmaceutical companies are disincentivized from investing in this field, since the estimated cost of developing a new antibiotic outweighs its expected revenue. “Capitalist pharma is not working for antibiotics, even in industrialized countries. It’s a broken system,” Nagel says.
The PASTEUR Act would introduce a subscription model wherein the U.S. government funds antimicrobial drug development. It would meaningfully shake up the status quo, since multinational pharmaceutical companies mainly reside in North America, Europe, and Japan. But it still might not be enough. When solutions are imported, Nagel says, they’re oftentimes not done so equitably, and don’t fit the needs of developing nations. Two billion people around the world—many of them in low- and middle-income countries—don’t have access to essential medicine.
“There are so many examples of drugs or medical devices that were developed from overseas that were never really taken up because they weren’t appropriate or weren’t trusted,” she says. The rollout of COVID-19 vaccines, for example, “was pretty pathetic” to low- and middle-income countries, as high-income countries skipped the line, causing delays of up to 100 days in vaccine delivery elsewhere. Even when doses of vaccines made it to these countries, their design introduced unanticipated logistical challenges. “Think of the COVID vaccines that required minus-80 refrigeration,” Nagel adds. That made them not quite as useful for developing nations without sophisticated cold chains in place.
In-country manufacturing could be key to bridging the divide between production and need, says Nagel, and there’s no better place to start than with phages. Unlike other antimicrobials, they require little more than a basic laboratory setup to research. Phages for Global Health aims to plant the seeds of a phage manufacturing sector in the developing world with workshops and international partnerships that empower and democratize the tools of local drug development. Their modest beginnings are already starting to bear fruit a decade later: 93 participants who completed workshops before the pandemic have taught the basics of phage biology to 1200 others. They’ve started over 50 research projects, and have earned over $1 million in research grants.
Nagel, who for years worked in the pharmaceutical industry for companies like Genentech and Novartis, feels that successful, large-scale phage therapy is inherently incompatible with a for-profit business model. Paul Garofolo, the Locus Biosciences CEO, wants to prove her wrong.
To him, the system isn’t the problem—it’s the finicky, mutable nature of phages that’s standing in the way. “If you want to address millions of infections, you need a fixed product,” he says.
Evolution (the delicate dance between phages and bacteria) has hampered clinical phage therapy on two counts. Evolutionarily speaking, a phage that can infect a bacterium but keep it alive can make more copies of itself than one that comes in and obliterates an entire colony. This leads to a changing product that isn’t optimized for killing bacteria. And cultured phages naturally change over time, thanks to natural selection and random genetic drift. Within a year or less, the exact same culture may contain a significantly different population of phages than it once did.
These two features would make any potential phage therapy unscalable, Garofolo argues, but it’s clear that the system of identifying a perfect cocktail of phages for an individual under compassionate use won’t work either. Locus, in contrast, is leading clinical trials for some bacterial infections that are fairly homogeneous across patients, obviating the need to reinvent the wheel each time. For instance, the company collaborated with Janssen Pharmaceuticals in 2019 to manufacture phage products, including one for antibiotic-resistant Pseudomonas aeruginosa. They took thousands of bacterial samples from patients, finding that 308 different isolates accounted for 95% of the genetic diversity among these infections. Locus then created one cocktail to target all these isolates, rather than optimizing cocktails for each individual isolate.
“If we have a panel that has 308 isolates in it, and then we have a cocktail of phage that can routinely infect more than 95% of that 308 panel, we have a drug that’s comparable to the standard of care,” Garofolo says.
Locus’ approach seems to be paying off. One product, a phage therapy cocktail for urinary tract infections caused by E. coli, is undergoing a Phase 2/3 clinical trial. Another “is knocking on the door” of clinical trials. Garofolo estimates that two more phage products will be ready within the next two years.
Getting Big
In “Phage Therapy in the Year 2035,” Pirnay’s patient survives the infection after printing a synthetic phage that clears out his pathogen. His life-threatening illness had been identified and treated within the comfort of his own home, dispelling any lingering uncertainty about the utility of phage therapy. But, it had not always been this way. As Pirnay wrote, adopting a reflective stance from the year 2035: “The medical world had taken a while to realize that phage therapy did not need to be identical to antibiotic therapy.”
Locus is attempting to turn a profit before it revolutionizes phage therapy as we know it. Still, Garofolo envisions a not-so distant future where the tools of synthetic biology shake up the basic science to create shelf-stable, hyper-effective phages. He says researchers could begin freeze-drying phage cocktails (a process known as lyophilization) as soon as Locus gets approval on a liquid drug. The process, in theory, would prevent co-evolution and genetic drift by suspending phages in a shelf-stable formula. Eventually, bacteria may still evolve to evade a fixed cocktail, but it’s unclear how many years that would take. Regulators have signaled that they would allow a phage therapy cocktail “to drift with the drift of the bacteria,” Garofolo says, letting manufacturers swap out individual phage components as they become out-of-date.
Exchanging phages in and out of a cocktail would be consequential for the business side of antimicrobial development, too. In contrast to the (widely ridiculed) Big Pharma tactic of “evergreening” drug patents by making small, immaterial tweaks to a product, these changes would materially change the composition of a phage therapy cocktail. The technique would then extend a manufacturer’s exclusivity on a drug patent, allowing a company to profit off the innovation indefinitely. With few economic incentives for the pharmaceutical industry to develop antibiotics, such a compensation scheme might make manufacturing phage therapy more appealing, though the social consequences are harder to predict.
Of course, Locus’ strategy of engineering phage cocktails for the most common bacterial infections is unlikely to work for every antibiotic-resistant infection. In lieu of mass production, groups like Phage Directory are trying to ensure that no patient gets left behind, no matter how complex or rare their infection is.
Still, this process is taking a toll on the researchers who are its biggest advocates. Scientists whose most stressful moments previously consisted of submitting grant applications and running time-intensive experiments now feel the weight of human lives riding on their ability to find suitable phages.
“We haven’t optimized it at all. We’ve barely had time to even sleep,” says Sacher, who works part-time on a clinical phage therapy service. Delivering phage therapy from the bench to the bedside is expensive: she estimates costs the equivalent of nearly $34,000 per patient.
The hyper-personalized nature of phage therapy that makes it so appealing for individual patients is what makes it so difficult to implement at scale, Sacher says. It’s one of the reasons why the implicit regulatory comparison often drawn between phages and antibiotics can set phage therapy up for failure, and why phage therapy clinical trials have borne out mixed results. For these reasons, her priorities lie outside a regulatory pathway for phage therapy.
“I’m not personally interested in fighting the fight of getting phages through the clinical trial system,” she says. “I would love to hold them to the same rigor as antibiotics, but people are dying in the process.”